Peer supervision is when therapists discuss their cases, seek feedback, share experiences, and provide mutual support in a structured and confidential setting. This collaborative approach enhances the quality of therapeutic interventions and fosters a culture of continuous learning and growth among practitioners.
Understanding Peer Supervision
Peer supervision is a process of collaboration, transparency, and reflexivity. Unlike traditional hierarchical supervision models where a senior clinician oversees the work of junior colleagues, peer supervision encourages equality and shared responsibility among participants. This egalitarian ethos creates a safe space where therapists can openly explore challenges, uncertainties, and successes without fear of judgment.

Key Components of Peer Supervision:
- Case Consultation: Participants bring forth challenging cases they are currently working on. Through a process of structured discussion, peers offer insights, alternative perspectives, and constructive feedback, enriching the therapist’s understanding and approach to the case.
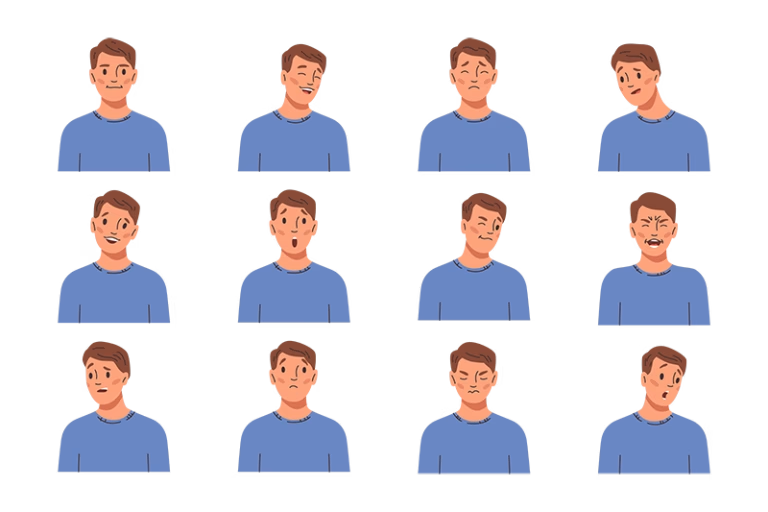
- Reflective Practice: Peer supervision encourages therapists to engage in reflective exercises, examining their own thoughts, feelings, and reactions towards clients and their presenting issues. This self-awareness is crucial for maintaining therapeutic boundaries and addressing countertransference.
- Skill Development: Participants have the opportunity to sharpen their clinical skills by observing and learning from the diverse approaches and techniques employed by their peers. This exposure to varied therapeutic modalities enriches their professional repertoire and fosters innovation.
- Emotional Support: Working in the field of therapy can be emotionally demanding. Peer supervision offers a supportive environment where therapists can share their struggles, vulnerabilities, and successes with colleagues who truly understand the nuances of their work.
Confidentiality Considerations
Confidentiality lies at the heart of effective peer supervision. Therapists must adhere to strict ethical guidelines to safeguard the privacy and dignity of their clients. Here are some key confidentiality considerations:
- Anonymity: When discussing cases, therapists should ensure that identifying details are anonymized to protect clients’ privacy. Refrain from using real names or any information that could lead to the identification of individuals.
- Informed Consent: Therapists must obtain informed consent from clients before discussing their cases. Clients should be informed about the purpose of peer consultation and assured that their confidentiality will be upheld.
- Boundaries: Establishing clear boundaries regarding sharing confidential information discussed is essential. Information shared within the supervision group should not be disclosed outside of that context without explicit consent.
- Documentation: While peer supervision discussions are confidential, therapists should maintain accurate records of the topics discussed and any agreed-upon recommendations or actions. These records should be stored securely and in compliance with relevant data protection regulations.
In conclusion, peer supervision is crucial for the development and ethical practice of therapy. By fostering collaboration, reflection, and support among peers, therapists can enhance their clinical skills, promote ethical conduct, and ultimately provide more effective care to their clients. However, it is crucial to uphold strict confidentiality standards to protect the privacy and dignity of those seeking therapeutic support.
Ready to begin? Start your online therapy journey today. Book your first session now.